Meaningful Use Stage 3: First Look
Meaningful Use of electronic health records (EHR) began as a goal of the 2009 Hitech Act. Healthcare providers were instructed to not simply adopt EHR, but to leverage EHR as a tool for improved efficiency and, ultimately, superior patient care. A total of $30 billion in incentives is to be paid out to providers who meet the government’s requirements for Meaningful Use. The requirements were divided into three stages. Stage 1 was implemented in 2011-2012 and focused on capturing and sharing patient data. Stage 2, started in 2014, focused on advancing clinical processes. On March 20, 2015, the Centers for Medicare and Medicaid Services (CMS) released the proposed rule for Stage 3.
The primary goal of Stage 3 criteria is for healthcare providers to achieve improved patient outcomes through EHR use. Below is a summary of the proposed rule’s requirements by category: patient engagement, system interoperability, and computerization of processes.
Patient Engagement
One major issue healthcare providers have faced, both historically and in the contemporary care setting, is a lack of patient engagement. Patients don’t participate in their own care to the extent that they could. They are passive, in many cases unaware of their own health patterns, the cause/effect links of their conditions, and even how to effectively follow their treatment plans. The proposed Stage 3 Meaningful Use criteria includes several measures that aim to more fully engage patients, such as:
- More than 25% of a healthcare provider’s patients must actively engage with their electronic health records. ‘Actively engaging’ can consist of either viewing, downloading or transmitting data from their records. This is a 20% jump from Stage 2 requirements, where only 5% of patients had to engage with EHR. Under Stage 3, however, providers are permitted to use an application programming interface (API) allowing third-party developers to access data for patients.
- After visiting a healthcare provider or hospital, more than 25% of patients must receive a message via the EHR’s secure messaging Messages must be clinically relevant, that is, they must relate directly to the patient’s visit. Responses from healthcare providers to messages initiated by patients also count towards fulfilling this requirement. Stage 2 required only 5% of patients to exchange messages with providers, making for another significant increase in this area.
- For more than 15% of patients, patient-generated data from a non-clinical setting must be collected and incorporated into the EHR. This data could come from health-related apps on mobile phones or wearable devices such as Fitbits. Information about daily exercise, diet, sleep, and other habits can give physicians tremendous insight into patient health patterns, and can help physicians pre-emptively recommend lifestyle changes for improved patient health. This is a new requirement in Stage 3, as Stage 2 did not include any criteria around patient-generated health data.
System Interoperability
Along with increasing patient engagement, the proposed Stage 3 requirements also aim to make it easier for physicians using different EHR systems to exchange patient information with one another. After all, what purpose would advanced EHR use serve if, after going to one healthcare provider, patients had to start all over again with the next provider they see? Time can be saved and unnecessary repetitions avoided if physicians using different systems are able to clearly and seamlessly communicate information to one another. With this goal in mind, proposed Stage 3 rules require that:
- For more than 50% of transitions of care and referrals, providers must use their EHR to create a summary of care to exchange electronically with other providers.
- In more than 40% of these transitions of care, providers must incorporate a summary of care from an EHR used by a different provider.
- For more than 80% of transitions of care, providers must perform a clinical information reconciliation. The reconciliation should include information about a patient’s medications and allergies, as well as problem lists.
Computerizing Processes
A third point of emphasis of the Stage 3 requirements is continued computerization of routine processes performed by physicians. With dozens of prescriptions being written every day, lab tests constantly being sent and received, and other fundamental information needing to be captured and stored, it’s in everyone’s best interest to get these processes flowing electronically rather than on paper. To that end, Stage 3 rules call for:
- 80% of prescriptions to be sent electronically. This is a 20% increase from Stage 2, which required physicians to send 60% of prescriptions electronically.
- 60% of lab and imaging orders to be sent electronically. This requirement doubles the existing percentage requirements, which was 30% under Stage 2.
In addition to the above, Stage 3 also changes the Meaningful Use reporting period. According to the proposed rule, all providers will be required to report under a full calendar year cycle beginning in 2017. An exception will be made for providers attesting to the Medicaid meaningful use program for the first time.
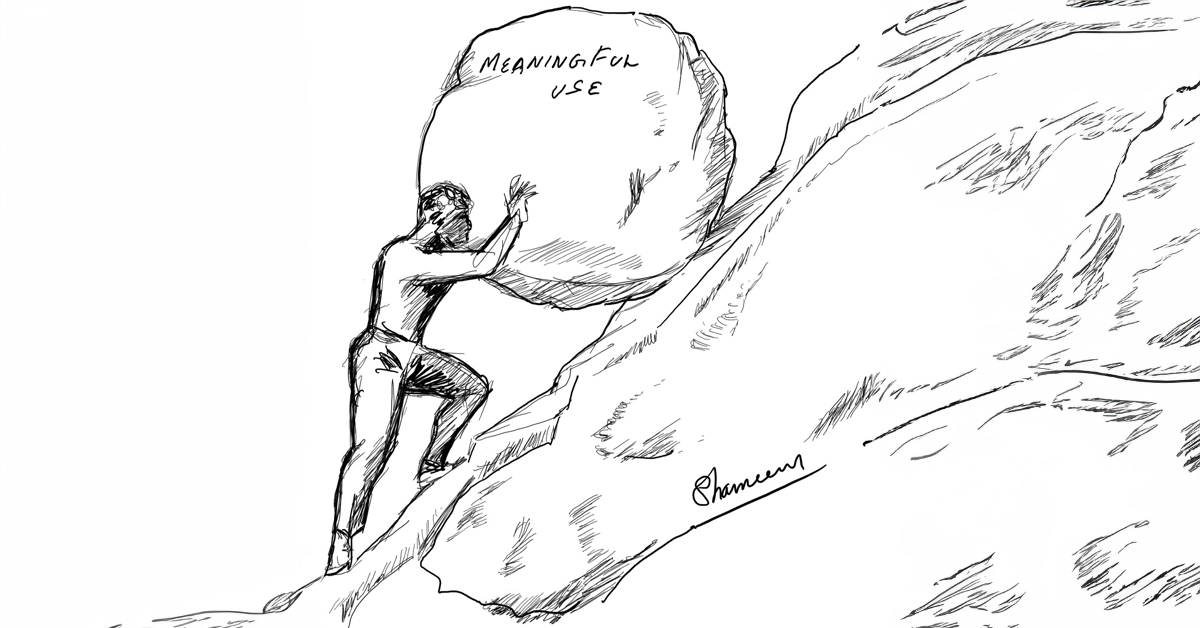
See below for a comparison of Stage 2 and Stage 3 Meaningful Use requirements.
| Requirement | Stage 2 | Stage 3 |
| Secure patient messages | 5% | 25% |
| Patients engaging with EHR | 5% | 25% |
| Patient-generated data | 0% | 15% |
| Electronic prescriptions | 60% | 80% |
| Electronic lab & imaging orders | 30% | 60% |
The Meaningful Use Stage 3 objectives are intended to support nationwide efforts to improve healthcare quality. The proposed rule is open for comments through May 29, 2015.